Spinal Decompression FAQs
Century Park Pain and Health Clinic Answers Common Questions
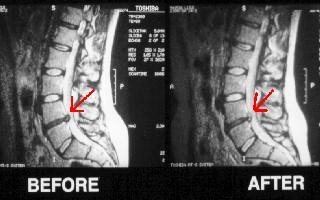
Spinal Decompression is a revolutionary new technology used primarily to treat disc injuries in the neck and in the low back.
What conditions does Spinal Decompression treat?
For lower back patients, the patient can be positioned on their back or stomach, which ever is more comfortable. This design is a unique feature of the Triton DTS table. Once positioned on the table, padded straps are used to securely fasten the patient to the table for treatment. For neck patients, the patient is put on there back in a semi-seated position where a soft rubber neck harness is used for the treatment. Once in place for the treatment the computerized equipment starts to pull in small increments, each being 20-30 seconds. By using small increments the body is allowed to relax into the treatment which allows the treatment to be more effective and more comfortable. Once the desired amount of tension is reached it is held for one minute followed by a 20-second interval of a decreased amount of tension (approximately half of the upper limit). This continues for 15-25 minutes and then is followed by a slow incremental lowering of tension until no tension is left on the patient.
Many patients have stated that it doesn’t feel like the table is pulling hard enough or that they can handle more, which tells us that it is doing its job properly. The less the patient feels with the appropriate amount of pull the more relaxed their body has become and the more effective the treatment is likely to be.
How does Spinal Decompression work?
The pumping action of the table does two things:
|
 |
Does Spinal Decompression work for all spinal conditions?
Typically, we see dramatic improvements with:
- Sciatica (pain or pins and needles radiating down one or both legs)
- Radiating neck pain (pain or pins and needles radiating down to shoulders, arms or into hands)
Very good improvements are seen in:
- Chronic neck pain
- Chronic low back pain
Tougher cases, such as spinal stenosis or patients with significant bone spuring, our success rates are a bit lower but still higher than a lot of the other options out there.
The most important part to remember is that we will evaluate you and give you options. If we don’t think we can help you, we will tell you and try to find an alternate solution.
Does insurance cover any of this treatment?
Is there any research on the effectiveness of Spinal Decompression?
There are several tables that perform non-surgical decompression of the spine. The following results were obtained from DRS/Inter-Discal Decompression (IDD) therapy, Vertebral-Axial Decompression and non-surgical Spinal Decompression Therapy. Although the concept of non-surgical Spinal Decompression therapy is similar in the DRS/VAX-D, please note that each table is a registered trademark and the following research may be specific to a specific decompression table/protocol employed.
Clinical Trials:
In a recent journal article in Orthopedic Technology Review titled Surgical Alternatives: Spinal Decompression, results showed that 86% of the 219 patients who completed the therapy reported resolution of symptoms while 84% of patients remained pain free 90 days post treatment. Physical examination findings showed improvement in 92% of the 219 patients, and remained intact in 89% of these patients 90 days after treatment.
Another article in Journal of Neurological Research reported that vertebral axial [spinal] decompression was successful in 71% of the 778 cases”. The success rate varied from 73% for patients with a single herniated disc. It was 72% for people with multiple herniated discs.
The American Journal of Pain Management reported “good to excellent” relief in 86% of patients with herniated discs, with back pain and sciatica symptoms being relieved. Good to excellent results were also obtained in 75% of those with facet syndrome.
A small non-randomized study in Anaesthesiology News reported of the 23 patients who responded to therapy, 52% had a pain level of zero, 91% were able to resume their normal daily activities, and 87% were either working or were retired without having back pain as the cause of retirement.
In a small study to determine the long-term effects of vertebral axial decompression, the following results were obtained: “Among 23 patients, 71% showed more than 50% reduction in pain immediately after treatment, and 86% showed a 50% or better pain reduction at four years. After four years, 52% of respondents reported a pain level of zero. Thus, pain relief not only improved but lasted. This pilot study shows great promise for long term relief and new pain management techniques.
An interesting study at the Rio Grande Hospital, Department of Neurosurgery compared the effects of 20 treatment sessions vs. 10 treatment sessions on chronic low back pain sufferers. The group receiving 20 treatments of decompression therapy reported a 76.5% with complete remission and 19.6% with partial remission of pain and disability. The second group, receiving 10 treatments of decompression therapy, reported a 42.9% rate of remission and 24.1% with partial remission. Failure rate was only 3.9% for those receiving 20 treatment sessions while it was 32.9% for those receiving only 10 sessions. Remission was defined as 90% or greater relief of pain, back to work without limitations, and abilities to carry out Activities of Daily Living (ADL’s). Partial remission was defined as persistence of some pain but ability to carry out most ADL’s and return to work with some restriction of duties, depending on the occupation. Failure rate was defined as no change in the level of pain and or/ADL.
As you can see from the above referenced Clinical Trials, Spinal Decompression Therapy is an effective therapy for people experiencing Discogenic or Arthritic pain (pain arising from the disc or caused by various types of Spinal Arthritis). In addition, promising research suggests that the effects of Spinal Decompression Therapy can be a long-lasting solution to certain chronic back pain disorders. Although failure rates are relatively low, studies suggest that completion of prescribed treatments can reduce failure rates from 32.9% to 3.9%.
What if it doesn’t work or I’m not a candidate for this kind of treatment?
How is Spinal Decompression different from standard traction or an inversion table?
Various forms of traction have been around for over 1000 years, however, pain relief has been inconsistent and short-lived with past techniques. In fact, several clinical studies have shown traction to be an ineffective form of back and neck pain relief. The reason is unexpected, but pretty simple. Our bodies react to the static unloading (stretching) of the spine by contracting, or squeezing, the muscles surrounding the spine. Rather than achieving the desired effect of unloading the spine, the pressure on the spine is actually increased, thus increasing intradiscal pressure (pressure on the discs). This does NOT allow the discs to rehydrate and heal, which is what ultimately yields pain relief.
Spinal Decompression, on the other hand, is a modified, updated form of traction. Computer technology is used to control variations in the unloading of the spine, effectively avoiding the body’s muscle contraction response. Notice in the figure below that the traction tension is varied over time according to the graph. The doctor can control how many progressive tension steps are experienced by the patient before reaching the maximum tension. The doctor also has complete control over how long the tensions are held steady and how often they are repeated.
Because Spinal Decompression avoids the muscle contraction response, the intradiscal pressure is actually lowered to the point of being a vacuum, creating a negative pressure. This vacuum is what allows herniated material to be drawn back into place and permits rehydration of the disc. Once the herniated material is not in contact with the nerves and the disc is in good health, pain is relieved. Spinal decompression is different from traction because it works. If you would like a more detailed comparison of traction and spinal decompression, please reference the clinical studies listed on our website specifically the following study. (Decompression, Reduction and Stabilization of the Lumbar Spine: A Cost-Effective Treatment for Lumbosacral Pain C. Norman Shealy, MD, PhD, and Vera Borgmeyer, RN, MA American Journal of Pain Management Vol. 7 No. 2 April 1997 Emerging Technologies: Preliminary Findings)
How do various Spinal Decompression tables compare?
 For instance, tables that support the patient under the arms have been reported to be much less comfortable, even causing injury to the shoulders and surrounding structures. Traction support under the arms does not permit the unloading to take place only at the specific problem area of the spine, unlike the Trition DTS belting system which can be very specific, if positioned properly. Furthermore, many of the tables that support under the arms do not allow the patient to be positioned in the prone (face down) position. For lumber injuries, many experts agree that the prone position, compared to the face-up position, allows the unloading of the spine to be even more specific and effective for the problem area.
For instance, tables that support the patient under the arms have been reported to be much less comfortable, even causing injury to the shoulders and surrounding structures. Traction support under the arms does not permit the unloading to take place only at the specific problem area of the spine, unlike the Trition DTS belting system which can be very specific, if positioned properly. Furthermore, many of the tables that support under the arms do not allow the patient to be positioned in the prone (face down) position. For lumber injuries, many experts agree that the prone position, compared to the face-up position, allows the unloading of the spine to be even more specific and effective for the problem area.
Is the Triton DTS as good as other tables such as the DRX-9000 or the VAX-D. Consider the fact that the Triton DTS and the DRX-9000 have the exact same FDA classification. Some tables market themselves as “the only true Spinal Decompression” or the only FDA-approved Spinal Decompression. Is this true? Well you can decide. Please see the attached FDA documents for both the Triton DTS and the DRX-9000 to compare for yourself. With all of that stated, patients find our office to have the expertise, equipment and professionalism to get the desired result from our therapies.
How does Spinal Decompression compare with surgical options?
Spinal Decompression is keeping a significant number of surgical candidates from ever having surgery. It doesn’t help everyone, but the outstanding clinical results, as well as the results we have seen in our office, are difficult to ignore. It is responsible to weigh the safety and success rates of different treatments. Studies have shown the efficacy of spinal surgery to be around 50% (depending on the severity of the condition and the skill of the surgeon). As well, one must take into consideration the lengthy recovery time involved post-surgery – often resulting in missed work and decreased quality of life. Compare that to the studies above (70-90% effective) and you will see that the conservative, non-surgical approach used with spinal decompression is an efficient form of treatment for those patients who are good candidates and should likely be tried before surgery as it is much less invasive.
Get Started Today
Contact Century Park Pain and Health Clinic now to schedule an appointment with Dr. Daniel Bateman.
CONTACT US »
